If you have a PPO Plus Premier plan and visit a dentist in our PPO network, you may have lower out-of-pocket costs. Members will be subject to balance billing for covered services. PPO Dentist : Coverage percent is based on the PPO Schedule of Fees. Premier : Coverage percent is based on the Participating Dentist Maximum Approved Charge (PMAC).
Non-participating: Coverage percent is based on the Non-Participating Dentist Maximum Approved Charge (NMAC). For greatest flexibility, members can choose a dentist in our Premier network, which includes three out of four dentists in the country and of dentists in Massachusetts. For greatest value, members can choose a dentist in our PPO network, which includes of Massachusetts dentists. Follow our simple, three-step registration process and to our secure system to see your eligibility information and benefits details. Best Dental Insurance Companies.
Prophylaxes (cleanings) are payable twice per benefit year and full mouth debridement is payable once in a five year period. Fluoride treatments are payable twice per benefit year for people up to age 19. Coverage Year A Coverage Year is a 12-month period in which dedu ctibles and benefit maximums apply. Covered Person per Coverage Year subject to the coverage percentages identified above. Three out of four dentists nationwide participate in one or both of these networks.
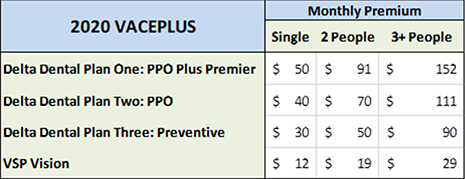
Summary of Dental Plan Benefits. Also eligible at your option are your legal spouse or domestic partner and your children who meet the age requirements noted above. You and your eligible dependents must enroll for a minimum of months.
The information shown here is not a guarantee of payment. Refer to the Certificate of Coverage for the full plan terms. This is a summary of benefits. The Certificate includes any limitations or exclusions not seen here.
Members have access to two of the nation’s largest networks. Delta Dental pays (called balance-billing). For services received out -ofnetwork, yourcosts will be greater. Nonparticipating dentists are paid at a reduced level.
A Dental Health Maintenance Organization Plan with no deductibles or dollar limits. Services must be obtained from an in-Network provider. Out- of -Network services are only covered in emergency situations. Benefit Options offers two dental plan options.

By encouraging preventive care, this dental program is designed to help contain dental costs. Dentist Reimbursement by Plan PPO : Ina Classic or OPTIONS PPO plan, all dentists ( PPO , Premier , and Non-contracted) are reimbursed at the lesser of the submitted charge or the PPO provider’s contracted fee. ABOUT HIS OR HER NETWORK PARTICIPATION STATUS WITHIN THE DELTA DENTAL PPO AND DELTA DENTAL PREMIER NETWORKS PRIOR TO RECEIVING DENTAL CARE.
If you or a family member need dental work you didn’t plan on, a supplemental dental plan can help reduce the amount you pay. After you have satisfied the deductible, if any, your dental program pays the following percentages of the treatment cost, up to a maximum fee per procedure. Whether you have a PPO or Premier dental plan, accessing in-network dental care is easy.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.